I. INTRODUCTION
In a hot spot of dioxin contamination around Da Nang Airbase, Vietnam, we have reported the effects of perinatal dioxin exposure indicated by dioxins in breast milk on neurodevelopment of infants and children at various ages until 5 years old. Particularly, in the first 3 years of life, associations between increased toxic equivalent (TEQ) levels of polychlorinated dibenzo-p-dioxins and polychlorinated dibenzofurans (PCDD/Fs) and decreased neurodevelopmental scores were observed in boys (Pham et al, 2016). In these subjects in Da Nang, TEQ-PCDD/Fs levels in breast milk were 4 times higher than those in non-sprayed areas, but contribution of 2,3,7,8-tetraclorinated dibenzo-p- dioxins (TCDD) was not high (around 10%; Pham et al, 2011), suggesting contamination in Da Nang was originated not only from agent orange, but also other herbicides. In contrast, contribution of TCDD was high (more than 25%) in another dioxin hot spot around Bien Hoa airbase in Vietnam (Nghi et al, 2015), suggesting Bien Hoa area is contaminated from agent orange more than Da Nang area. However, the effects of dioxins on their neurodevelopment under 3 years old in Bien Hoa is not severe as that in Da Nang. Therefore, in this study, we reviewed our previous studies and compared dioxin effects on neurodevelopment and behaviour between two hot spots of dioxin contamination in Vietnam.
 |
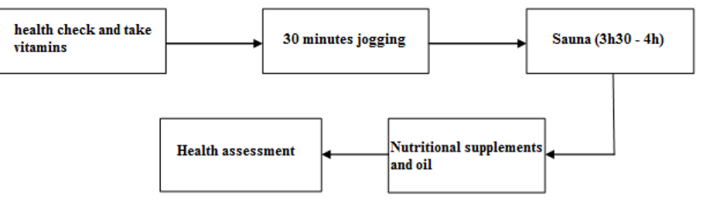
II. METHODS
In 2008 and 2009, total 241 mother-infant pairs in the Thanh Khe and Son Tra district in Da Nang were enrolled in the present study. When the pregnant mothers gave birth in these 2 district hospitals, obstetricians recruited them on the basis of some criteria.
The subjects were followed up at various ages: 1 and 4 months of age, 1 year, 3 years and 5 years of age. Effects of dioxin on development of these children since birth until 5 years old had been examined using standardized neurodevelopmental scales and behavior rating scales. A total of 227 children in an exposed area in Bien Hoa in southern Vietnam were recruited in 2012 and 2015 in Dong Nai Hospital and participated to the followed up survey at 6 months and 2 years of age. These children in Bien Hoa were also examined using same neurodevelopmental scales.
Breast milk samples were collected from mothers one month after birth and dioxin levels in breast milk were measured using GC-HRMS (JEOL Ltd.) in Kanazawa Medical University, and used as perinatal exposure markers to children. Geometrical means (GMs) of TCDD in breast milk were 1.4 (pg/g lipid) in Da Nang, and 2.1 (pg/g lipid) in Bien Hoa. Neurodevelopmental and behavior scores of participants was compared among exposure groups with different TCDD and TEQ-PCDD/Fs levels in breast milk after adjusting age, education years, parity (primiparae or multiparae), and drinking habit during pregnancy of mothers, family income, family smoking, and gestational weeks, birth weight, and age at the survey of children.
III. RESULTS
3.1. Follow-up studies of Vietnamese birth cohort in Da Nang
Associations perinatal dioxin exposure indicated by dioxin isomers including TCDD and TEQ-PCDD/Fs in breast milk and neurodevelopmental scores tested using the Bayley scales of infant and Toddler development, third edition (Bayley-III) were reported at 4 months of age (Tai et al, 2013). Although we found no association between TCDD exposure and Bayley-III scores in the Da Nang cohort of 3-year-old children, Bayley-III scores in all domains significantly decreased in the high-TEQ-PCDD/Fs exposure group in boys (Nishijo et al, 2014). Consistent with these findings in the cross sectional survey at 3 year of age, decreased expressive language scores and motor scores in boys were found in the 3-year longitudinal follow-up study of this Da Nang cohort (Tai et al, 2016).
In the cross-sectional survey at 3 years of age in Da Nang, we reported increased autistic behaviour associated with increasing TCDD exposure at 3 years of age (Nishijo et al, 2014) in both sexes. In the same cohort in Da Nang, we investigated alteration of eating behavior using Child Eating Behavior Questionnaire and reported that high levels of TEQ-PCDFs and TEQ-PCDD/Fs were associated with a reduction in eating behaviour for food approach in girls (CEBQ; Anh et al. 2018). Also, we previously reported poor coordination movement skills at 5-year-old boys in Da Nang cohort (Nghi et al, 2015) associated with TEQ-PCDD/Fs exposure which are often found in children with autism spectrum disorders.
3.2. A follow-up study of Vietnamese birth cohort in Bien Hoa
In birth cohort in Bien Hoa, adjusted mean of Bayley express language score at 2 years of age was significantly decreased in the highest TCDD group (> 5.5) in boys, compared with controls in Ha Dong. Gross motor scores were significantly lower compared with controls, but there was no dose-effect relationship between TCDD exposure and gross motor scores. In girls, adjusted mean of gross motor scores was significantly lower in the highest TCDD group. Composite motor scores in all 3 TCDD exposure groups were significantly lower in girls, but no dose-effect relationship was observed between them. However, no significant decreased Bayley score compared with controls was found in the highest TEQ-PCDD/Fs exposure group in both sexes. Therefore, these results indicate that perinatal high TCDD exposure originated from Agent Orange, not TEQ-PCDD/Fs, may influence neurodevelopment in boys and girls at the 2 years of age in sex different manner.
3.3. Comparisons of neurodevelopmental and behavioral effects of dioxins between Da Nang and Bien Hoa
Comparing the Bayley-III scores between the Bien Hoa (TCDD dominant area) and Da Nang (TEQ-PCDD/Fs area), we found some differences in the effects of dioxin exposure on neurodevelopment between 2 areas; 1) TCDD effects on Bayley III scores in Bien Hoa and TEQ-PCDD/Fs effects on Bayley III scores in Da Nang; 2) the effects were found in both sexes in Bien Hoa and mainly boys in Da Nang; 3) TCDD exposure influence on child behaviour in Da Nang, but effects of dioxins on behaviour still unsettled in Bien Hoa.
IV. DISCUSSION
The effects of dioxin exposure on child neurodevelopment have been reported in several countries, with inconsistent findings. In a Dutch birth cohort exposed to dioxins and PCBs from industrial activities, infant development scores at 3 and 7 months of age were affected by the exposure, but no associations were detected at 18 months (Koopman-Esseboom et al, 1996). Similarly, in a German cohort, no association was found between dioxin exposure and neurodevelopmental scores at 2 years of age (Wilhelm et al, 2008). However, Dutch children 42 months of age and older exhibited decreased cognitive scores associated with perinatal exposure to dioxins and PCBs (Patandin et al, 1999; Vreugdenhil et al, 2002). Similarly, a Norwegian cohort exhibited an inverse association between dioxin and PCB exposure during pregnancy and language development in children aged 3 and a half years, with significant effects observed only in girls (Caspersen et al, 2016). In the Faroe Islands (Denmark), prenatal PCB exposure (measured in cord blood) prolonged reaction time for naming objects in children aged 7 years (Grandjean et al, 2001).
These findings suggest that the effects of prenatal exposure to dioxins and PCBs on neurodevelopment may not be evident in early childhood but appear later. In addition, boys do not always exhibit these effects. In the Netherland, inverse associations between TEQ-PCDD/Fs levels in maternal blood and social responsiveness scale scores was also reported in children at 10 years of age in Duisburg cohort study (Nowack et al, 2015). Alteration of gender specific play behaviour and increased behaviours related to attention deficit hyperactivity disorder (ADHD) were also reported in Duisburg cohort at school age (Neugebauer et al, 2015). In addition, developmental milestone from 24 months have been reported to partly predict developmental outcome of children in childhood and adulthood (Murray et al, 2007; Peyre et al, 2017). Therefore, effects of TCDD exposure on expressive language and gross motor skills observed here in 2-year- old children might predict to psychiatric disorders including neurodevelopmental disorders such as autism spectrum disorders and ADHD in later childhood.
CONCLUSION
We need to follow-up these children in Bien Hoa and Da Nang to clarify dioxin effects on their neurodevelopment and behaviour until adolescent period.
Muneko Nishijo1; Pham Ngoc Thao1,2; Pham The Tai2; Vu Thi Hoa2; Hoang Van Luong2; Tran Hai Anh2'; Tran Ngoc Nghi3; Yoshikazu Nishino1 ;Hisao Nishijo4; Do Quyet2
1. Department of Public Health, Kanazawa Medical University, Ishikawa, Japan
2. Biomedical and Pharmaceutical Research Center, Vietnamese Military Medical University, Hanoi, Vietnam
3. Ministry of Health, Vietnamese Government, Hanoi, Vietnam
4. System Emotional Science, Graduate School of Medicine, University of Toyama, Toyama, Japan
REFERENCES
1. Pham The Tai, Nishijo M, Tran Ngoe Nghi, et al. (2016) ; J. Pediatr. 175:159-166
2. Pham The Tai, Nishijo M, Kido T, et al. (2011); Environ. Sci. Techno!. 45: 6625-6632
3. Tran Ngoe Nghi, Nishijo M, Ho DM, et al. (2015); Environ. Sci. Techno!. 49: 5732-5742
4. Pham The Tai, Nishijo, M., Nishijo, H., et al. (2013); Occup. Environ. Med. 70 : 656-662.
5. Nishijo M., Pham The Tai, Tran Hai Anh., et al. (2014); Mol. Psychiatry. 19, 1220-1226.
6. Nguyen Thi Nguyet Anh, Nishijo M, Pham The Tai, et al. (2018) ; BMC Pediatri 18(1):213
7. Tran, N.N., Pham, T.T., Ozawa, K„ et al. (2016) ; PLoS One. 11, e0147655.
8. Koopman-Esseboom, c., Weisglas-Kuperus, N., et al. (1996). Pediatrics. 97, 700-706.
9. Wilhelm, M., Wittsiepe, J., Lemm, F., et al. (2008) Mutat. Res. 659, 83-92.
10. Patandin, s., Panting, C.I., et al. (1999). J. Pediatr. 134, 33-41.
11. Vreugdenhil, H.J., Slijper, F.M., Mulder, P.G., et al. (2002). Environ. Health Perspect. 110, A593-598.
12. Caspersen, I.H., Aase, H., Biele, G., et al. (2016). Environ. Int. 94, 649-660.
13. Grandjean, p., Weihe, p., Burse, V.W., et al. (2001). Neurotoxicol Teratol. 23, 305-317.
14. Nowack, N., Wittsiepe, J., Kasper-Sonnenberg, M., et al. (2015). PLoS One. 10, eO129906
15. Neugebauer, J., Wittsiepe, J., Kaspèr-Sonnenberg, M., et al. (2015).. Int. J. Hyg. Environ. Health. 218, 153-162.
16. Murray, G.K., Jones, P.B., Kuh, D„ et al. (2007).. Ann. Neurol. 62, 128-136.
17. Peyre, H., Charkaluk, M.L., Forhan, A., et al. (2017). Eur. J. Paediatr. Neurol. 21, 272-279.



_thumb_720.jpg)







_thumb_720.jpg)




















Comment