The greatest wish of all parents is to give birth to a normal child who can grow up without any defects in any basic functions affecting life or learning later in life. of children. Today, to ensure a healthy baby is born, the identification of risk factors, the diagnosis of fetal abnormalities is done earlier and earlier, with many different methods. In general, prenatal diagnosis can be divided into two main groups: screening tests and diagnostic tests. Because birth defects in babies can be genetic (chromosomal or gene) or not, regardless of age, whether or not there is a history of abnormal births is recommended. screening and diagnostic tests, at least during pregnancy.
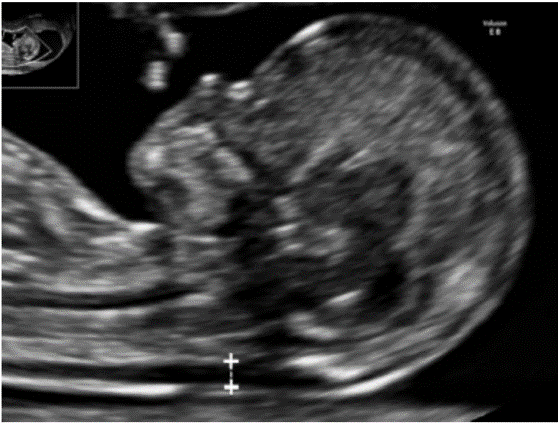
Ultrasound is the most commonly used routine test to screen for and diagnose abnormalities in pregnancy. With the advancement of science and technology, the development of imaging techniques such as high resolution, high frequency probes, so in addition to monitoring fetal development can diagnose fetal abnormalities, Birth defects, complications of pregnancy. The main purpose of ultrasound is to provide accurate information, to coordinate with clinicians to come up with appropriate monitoring and management options, to ensure the best outcome for mother and fetus.
Prenatal ultrasound is considered a safe technique. To date, there is no evidence that ultrasound harms the mother or the fetus or affects the growth and development of the fetus, nor is there evidence to increase the frequency of fetal death, fetal malformations, malignancies, and malignancies. also does not affect children's ability to read, write, learn math... [1, 2, 3]
2. CONTENT
2.1. The role of ultrasound in the first trimester of pregnancy
Ultrasound in the first trimester of pregnancy can help determine the fetal status (determine pregnancy or not), the position of the fetus (inside or outside the uterus), determine the fetus when the embryo has fetal heart activity, determine Gestational age (from 8 weeks to 14 weeks)
2.1.1. Survey on fetal morphology in the first trimester of pregnancy
Morphological ultrasound (evaluating external abnormalities) in the second trimester of pregnancy - from 18 to 22 weeks - is still the standard ultrasound to examine the morphological structures of the fetus. The first-trimester ultrasound to examine the morphology and screen for fetal abnormalities was applied in the late 1980s and early 1990s, with the effective aid of the ddaho transducer. After that, ultrasound measurement of nuchal translucency (MRG) from 11 to 13 +6 weeks was introduced, showing that the role of morphological ultrasound in the first trimester of pregnancy becomes practical. Fetal imaging at this stage helps in early detection and exclusion of major abnormalities, assessment of high-risk pregnancies, early diagnosis of genetic abnormalities and, if necessary, early termination of pregnancy.
2.1.2. Structures to be evaluated
 |
2.1.3. Some clinical cases:
 |
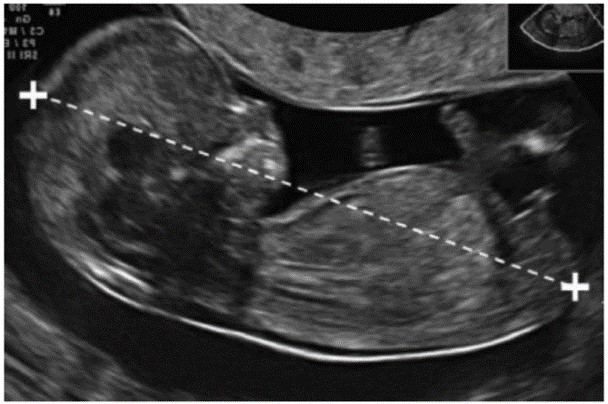
Brain parenchyma has no outer covering of the skull
Pregnancy stage 11-13, 6/7 weeks, the lateral ventricle is slightly large and is filled with 2/3 of the posterior horn by the choroid plexus. The two cerebral hemispheres are balanced and clearly separated by the sulcus and crescent of the brain. The corpus callosum is very thin, most clearly seen in the front, the ventricles are filled with fluid, so it should be distinguished from hydrocephalus. At this stage, some brain structures are not fully developed (such as the bottle, cerebellum) so they may not be visible.
Patient 13 weeks: first antenatal check-up found anencephaly
* The light at the back of the neck is thick:
The nuchal translucency (also known as nuchal translucency - NT) is an important part of screening for fetal chromosomal abnormalities.
 |
| Figure 2. The length of the rump (A) and the light at the back of the neck (B) |
(A) (B)
 |
| Figure 3. The light on the back of the neck at 12 weeks of pregnancy – Source: My Duc Hospital |
Light space after thick skin increases the risk of Down's syndrome
+ The frequency of Down's syndrome (Trisomy 21) increased 3 times when NT = 3mm; 18 times more when NT = 4mm, 28 times more when NT = 5mm, 36 times more when NT = 6mm(4).
+ Nasal bone: 73% of fetuses with Down syndrome do not see the nasal bone at 11-14 weeks of ultrasound. In contrast, up to 99.5% of normal fetal cases observed nasal bones (4).
| ||
+ Lymphatic cysts in the neck area. Source: My Duc Hospital
 |
| Figure 5. Thick back of the neck with umbilical hernia |
T.T.N – 27 years old- PARA 0000
* Hernia of the abdominal wall:
In the period 11-13 6/7 weeks, the stomach and bladder can be visualized, which is the empty echogenic structure in the abdomen. The fetal stomach is located on the left side, the intestines are in the abdomen and the umbilical cord is inserted into the abdominal wall. The fetal kidney is located next to the spine, has a structure resembling a pea.
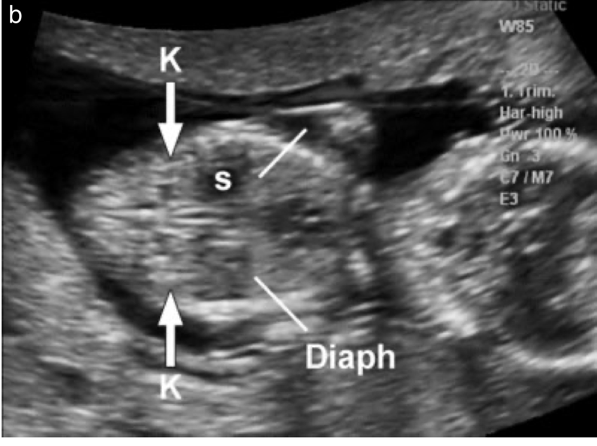 |
| Figure 6. Stomach and 2 kidneys of fetus |
2.2. Role of second trimester ultrasound
Ultrasound at this stage, in addition to monitoring fetal development, also helps detect birth defects. Although ultrasound can detect many malformations, some abnormalities can still be missed, even if the sonographer is experienced or has anomalies that appear late.
Second trimester ultrasound assesses fetal morphology in detail.
SOME CLINICAL CASES:
* Bilateral ventricular dilatation:
Patient N.T.T - 25 years old - History of 1 miscarriage - Natural pregnancy
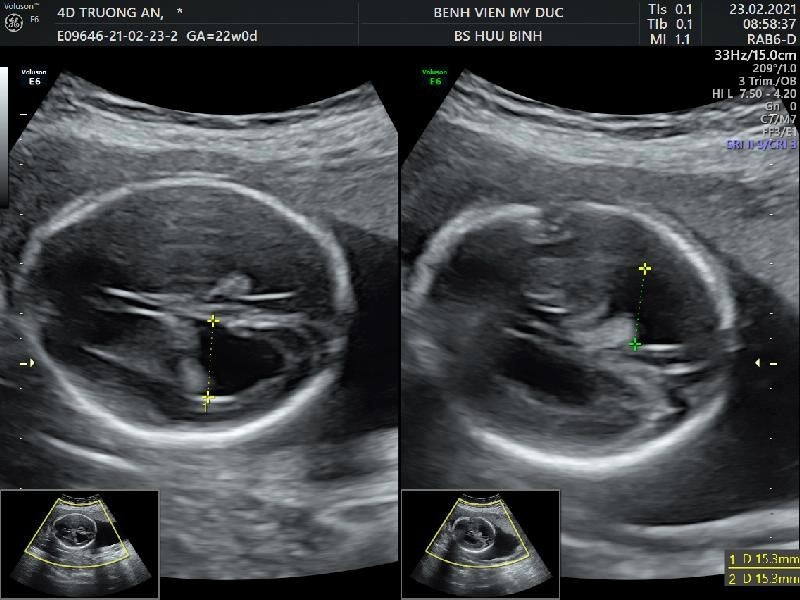 |
| Figure 7. Bilateral ventricular dilatation (diameter greater than 10mm) |
* Tumors next to the spine:
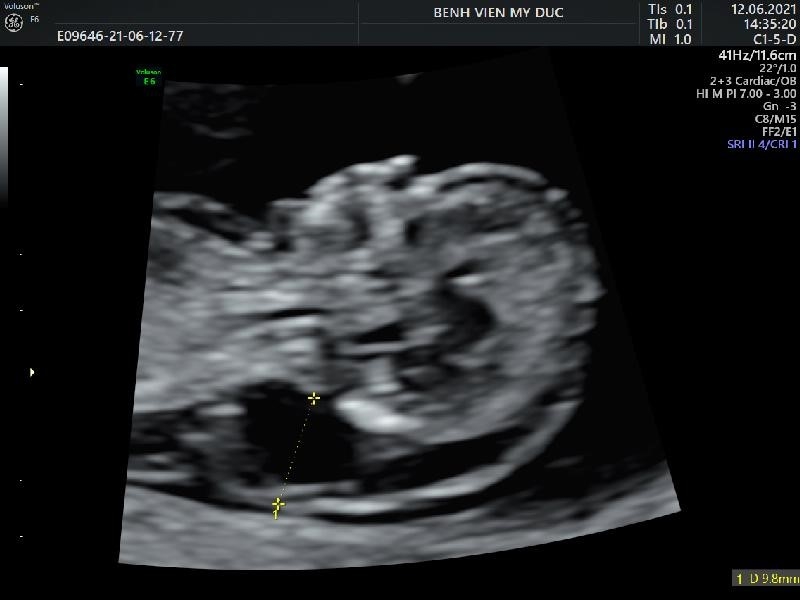
Patient: 26 years old – PARA: 0020 (2 early miscarriages) – Spontaneous pregnancy - Routine out-of-hospital antenatal check-up did not find any abnormalities
Ultrasound examination of morphology at 21 4/7 weeks at My Duc hospital recorded a paravertebral mass. MRI: Paravertebral mass has not ruled out Teratoma. The patient decided to monitor the pregnancy, during the follow-up, the tumor did not increase in size, and did not record any other abnormalities. The patient had a cesarean section when she was 38 weeks pregnant – The baby had surgery after 2 months, the tumor was benign. The baby is developing normally.
4D ultrasound – rendering: Tumor adjacent to the spine
(Source: My Duc Hospital).
* Tumor of sacral region - fetal amputation:
- Pregnancy after IVF – twins, a tumor suspected of teratoma (teratoma in the fetal sacrum).
 |
Tumor in the sacrum – fetal amputee – has invaded the pelvis
* Beckwith-Wiedemann syndrome:
- Patient 28 years old, PARA 0000 – Natural pregnancy.
- Ultrasound at 22 weeks recorded: big tongue, 2 big kidneys, thick placenta, big baby.
Image: thick placenta, large tongue, large kidneys on ultrasound.
- Baby after birth: cesarean section at 34 17/week – weight 3100g
- The placenta weighs 2500g – Baby died 4 days after birth due to infection
2.3. The role of ultrasound in the third trimester of pregnancy:
The third trimester of pregnancy mainly evaluates fetal growth, detects cases of fetal growth retardation to guide appropriate monitoring and evaluation of fetal health. Screening for malformations in the third trimester is less significant than in the second trimester. However, it can also help detect late or previously unrecognized malformations.
3. CONCLUSION
Thus, ultrasound in pregnancy plays an important role in screening and diagnosing fetal abnormalities, in order to intervene or manage the pregnancy appropriately. With the development of imaging techniques, screening and prenatal diagnosis, the rate of children with birth defects is decreasing, reducing the medical burden for the family, society, and for a future generation.
REFERENCES
Screening for fetal chromosomal abnormalities. ACOG Practice Bulletin No. 226. American College of Obstetricians and Gynecologists. Obstet Gynecol 2020;136.
Khalil A, Rodgers M, Baschat A, Bhide A. et al. (2016), ISUOG Practice Guidelines: role of ultrasound in twin pregnancy. Ultrasound Obstet Gynecol 2016; 47: 247 – 263.’
Salomon LJ, Alfirevic Z, Bilardo C. M. et al. (2013), ISUOG Practice Guidelines: performance of first-trimester fetal ultrasound scan. Ultrasound Obstet Gynecol 2013; 41: 102–113.’
L. J. Salomon, Z. Alfirevic V. Berghella, C. Bilardo et al. (2010), On Behalf Of The Isuog Clinical Standards Committee. Practice guidelines for performance of the routine mid-trimester fetal ultrasound scan. Ultrasound Obstet Gynecol (2010)
World Health Organization (2005), Report on the Regional Consul- tation Towards the Development of a Strategy for Optimizing Fetal Growth and Development. WHO Regional Office for the Eastern Mediterranean: Cairo, 2005.
































Comment